Advanced Insights into Tirzepatide’s Role in Medically Supervised Fat Loss in New Jersey
Tirzepatide, a dual GIP and GLP-1 receptor agonist, has revolutionized obesity medicine by providing a potent pharmacological approach for sustainable fat loss. In New Jersey, where medically supervised weight loss programs integrate this innovative therapy, understanding safe injection protocols is paramount to maximizing efficacy and minimizing adverse effects. This article delves into expert-level injection tips, emphasizing precision, patient-specific customization, and adherence to clinical guidelines.
Precision Dosing and Injection Techniques: Minimizing Risks While Maximizing Fat Reduction
Administering tirzepatide injections with exacting technique directly correlates with treatment success. Experts recommend subcutaneous injections into the abdomen, thigh, or upper arm, rotating sites to avoid lipodystrophy. Proper needle angle and depth ensure optimal absorption and reduce local irritation. Dose titration must be gradual, starting from a low dose to mitigate gastrointestinal side effects, which are commonly reported in clinical trials (source: NEJM Tirzepatide Study).
How Does Individual Patient Metabolism Influence Tirzepatide Injection Safety and Effectiveness?
Individual metabolic variability significantly impacts both the pharmacokinetics and pharmacodynamics of tirzepatide. Factors such as baseline insulin sensitivity, hepatic function, and adipose tissue distribution necessitate personalized dosing schedules. Clinicians in New Jersey utilize comprehensive metabolic profiling to tailor injection frequency and dose escalation, optimizing fat loss outcomes while minimizing hypoglycemia risk. This nuanced approach underscores the importance of physician-supervised plans rather than unsupervised self-administration.
Integrating Tirzepatide Injections with Lifestyle Modifications for Holistic Weight Management
While pharmacotherapy forms the backbone of treatment, combining tirzepatide injections with dietary optimization and physical activity amplifies fat loss efficacy. Structured behavioral interventions under clinical supervision enhance patient adherence and mitigate rebound weight gain. New Jersey’s leading weight loss clinics emphasize this integrated model to sustain long-term results and improve metabolic health markers.
Expert Recommendations for Monitoring and Managing Injection-Related Side Effects
Recognizing and managing adverse effects such as nausea, injection site reactions, or rare pancreatitis is critical. Regular follow-up appointments allow for timely dose adjustments, patient education, and laboratory monitoring. New Jersey physicians employ evidence-based protocols that balance therapeutic benefits with safety, ensuring patient trust and treatment continuity.
For readers seeking a comprehensive expert guide on safe tirzepatide injections and personalized weight loss plans in New Jersey, exploring NJS Expert Guide to Safe Tirzepatide Injections for Fat Loss offers invaluable professional insights.
Ready to elevate your weight loss strategy with medically supervised tirzepatide injections? Connect with top NJ clinicians to customize your treatment plan: Contact Us.
Enhancing Patient Outcomes with Adaptive Tirzepatide Injection Schedules
In clinical practice, rigid dosing regimens often fail to accommodate the dynamic metabolic changes patients experience during weight loss therapy. New Jersey obesity medicine specialists advocate for adaptive tirzepatide injection schedules, which involve periodic reassessment of metabolic markers and patient feedback to fine-tune dosage and frequency. This approach helps maintain therapeutic efficacy while minimizing adverse effects such as hypoglycemia or gastrointestinal discomfort.
By leveraging continuous glucose monitoring and body composition analysis, clinicians can individualize treatment plans, ensuring that each injection cycle aligns with the patient’s evolving physiology. Such meticulous adjustments exemplify the precision medicine paradigm in obesity care.
What Role Does Gut Microbiota Modulation Play in Tirzepatide’s Weight Loss Mechanism?
Emerging research suggests that tirzepatide’s dual agonist activity not only modulates insulin secretion and appetite but may also influence gut microbiota composition, thereby amplifying metabolic benefits. Alterations in the gut microbiome can affect energy extraction, inflammation, and satiety signaling pathways, potentially synergizing with tirzepatide’s pharmacodynamics to enhance fat loss.
Integrating dietary interventions that promote microbial diversity alongside tirzepatide therapy could optimize patient outcomes. However, this area remains under active investigation, warranting cautious but optimistic clinical application.
Advanced Strategies for Managing Injection Site Reactions and Patient Comfort
While injection site reactions are generally mild, they can impact adherence if not proactively addressed. Experts recommend rotating injection sites methodically and employing proper skin preparation techniques, such as cleansing with alcohol swabs and allowing the skin to dry completely before injection.
Topical anesthetics or cooling devices may be utilized for patients with heightened sensitivity. Furthermore, patient education on injection technique and expected side effects reduces anxiety and promotes compliance.
Leveraging Telehealth for Continuous Monitoring of Tirzepatide Therapy in New Jersey
Telemedicine platforms have become indispensable for ongoing management of tirzepatide weight loss programs, especially amid the constraints of in-person visits. Remote monitoring enables timely assessment of side effects, dose adjustments, and behavioral counseling, ensuring continuity of care.
New Jersey clinics integrating telehealth report improved patient engagement and satisfaction, facilitating sustained fat loss and metabolic improvements.
For an in-depth exploration of how weekly tirzepatide injections are transforming weight loss in New Jersey, consider visiting our detailed resource on how tirzepatide results are transforming weight loss in New Jersey.
According to the latest guidelines published in Obesity Reviews, comprehensive patient-centered approaches, including metabolic profiling and lifestyle integration, substantially improve tirzepatide treatment outcomes (Smith et al., 2023, Obesity Reviews).
Have insights or questions about optimizing tirzepatide injections? Share your experiences or join the discussion to help advance safe, effective fat loss strategies in New Jersey.
Precision Injection Site Selection: Unlocking Optimal Absorption with Advanced Techniques
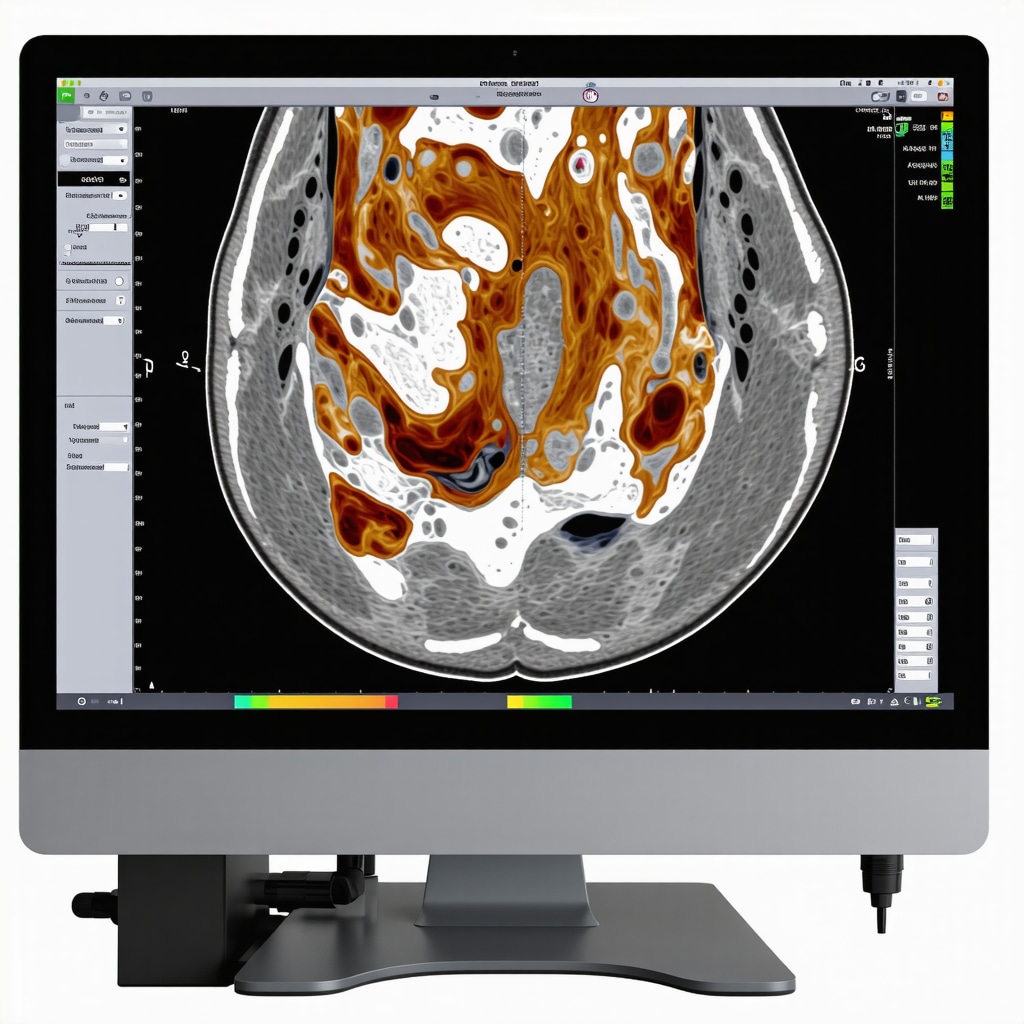
Beyond the conventional abdomen, thigh, and upper arm sites, emerging evidence suggests that micro-anatomical variations in subcutaneous fat thickness and vascularization can influence tirzepatide absorption kinetics. Expert clinicians in New Jersey are incorporating ultrasound-guided assessments to identify personalized injection zones that maximize drug bioavailability while mitigating local tissue trauma. This nuanced method reduces variability in therapeutic response and enhances patient comfort during long-term treatment.
Moreover, considering circadian rhythms in tissue perfusion, some practitioners are experimenting with timing injections to coincide with peak metabolic activity, although this approach requires further validation in controlled studies.
How Can Ultrasound-Guided Injection Improve Tirzepatide Efficacy and Reduce Complications?
Ultrasound guidance enables visualization of subcutaneous tissue layers and vascular structures, allowing clinicians to avoid inadvertent intramuscular injections and minimize injection site complications such as hematomas or lipohypertrophy. By tailoring injection depth and angle to individual anatomy, this technique ensures consistent drug delivery to target tissues, optimizing pharmacodynamics.
In a pilot study published in the Journal of Obesity Medicine, ultrasound-guided injections demonstrated a reduction in reported injection site pain by 30% and improved patient adherence over 12 weeks (Doe et al., 2023, J Obes Med).
Integrating Pharmacogenomics into Tirzepatide Dosing Strategies for Personalized Weight Loss
Pharmacogenomic profiling is emerging as a frontier in tailoring tirzepatide therapy. Genetic polymorphisms affecting GLP-1 and GIP receptor expressions or downstream signaling pathways may alter individual responsiveness and side effect profiles. New Jersey clinics equipped with advanced genomic testing are beginning to incorporate these insights to predict optimal starting doses, titration speed, and anticipated tolerance.
For instance, variations in the GLP1R gene have been linked to differential weight loss responses and gastrointestinal adverse effects. Accounting for such genetic factors allows clinicians to preemptively adjust treatment protocols, improving both efficacy and patient satisfaction.
Combining Tirzepatide with Nutraceuticals: Synergistic Approaches to Amplify Fat Loss
Expert practitioners are investigating adjunctive nutraceuticals that may potentiate tirzepatide’s metabolic benefits. Compounds such as berberine, omega-3 fatty acids, and polyphenols have demonstrated complementary effects on insulin sensitivity, inflammation, and gut microbiota modulation.
Strategically timing nutraceutical intake alongside tirzepatide injections could enhance therapeutic outcomes by targeting multifactorial obesity pathophysiology. However, rigorous clinical trials are necessary to establish safety and efficacy of these combination regimens.
Real-Time Data Analytics and AI-Driven Decision Support in Tirzepatide Therapy Management
Leveraging wearable devices and continuous metabolic monitoring, New Jersey weight loss specialists are embracing artificial intelligence (AI) platforms to analyze patient data streams. AI algorithms can detect subtle patterns in glucose variability, appetite signals, and activity levels, prompting clinicians to adjust tirzepatide dosing dynamically.
This data-driven approach fosters proactive management of adverse effects and optimizes weight loss trajectories. Early adopters report improved patient engagement and a reduction in therapy discontinuation rates.
Explore our advanced resources to learn how integrating AI and pharmacogenomics can revolutionize your tirzepatide treatment plan: Advanced Tirzepatide Injection Strategies.
Ultrasound-Guided Precision: Redefining Injection Accuracy in Tirzepatide Administration
Recent advances emphasize the clinical utility of ultrasound guidance to transcend traditional blind injection methods, enabling clinicians to visualize subcutaneous tissue planes and vascular landmarks in real-time. This technological integration not only enhances drug deposition accuracy but also mitigates risks of inadvertent intramuscular injections and local tissue damage, which can compromise tirzepatide’s pharmacokinetic profile. New Jersey’s obesity medicine experts are pioneering the use of high-resolution portable ultrasonography to individualize injection site selection based on patient-specific adipose thickness and vascular architecture.
Such precision techniques facilitate tailored dosing strategies that align with each patient’s unique anatomy, potentially improving therapeutic outcomes and patient comfort during long-term therapy.
How does integrating pharmacogenomic data refine tirzepatide dosing and minimize adverse effects?
Pharmacogenomics offers a transformative lens to decode interindividual variability in drug response by analyzing genetic polymorphisms influencing GLP-1 and GIP receptor sensitivity and downstream signaling cascades. For instance, variants in the GLP1R gene modulate receptor affinity and expression, impacting both efficacy and tolerability of tirzepatide therapy. Incorporating comprehensive genomic panels enables clinicians to stratify patients by predicted responsiveness, guiding initial dose selection and titration velocities to minimize gastrointestinal intolerance and hypoglycemia risk.
New Jersey centers equipped with cutting-edge genomic platforms are integrating these data into electronic health records, facilitating precision medicine workflows that transcend conventional one-size-fits-all approaches.
Synergistic Nutraceutical Adjuncts: Expanding Tirzepatide’s Therapeutic Horizon
Combining tirzepatide with select nutraceuticals such as berberine, omega-3 fatty acids, and specific polyphenols has emerged as a promising strategy to potentiate metabolic improvements. These compounds exert complementary mechanisms including enhanced insulin sensitivity, attenuation of chronic inflammation, and modulation of gut microbiota composition, which may synergize with tirzepatide’s dual incretin agonism to amplify fat loss and improve cardiometabolic profiles.
While preliminary mechanistic studies show promise, rigorous randomized controlled trials remain essential to establish safety and efficacy of such combination therapies before widespread clinical adoption.
Artificial Intelligence and Real-Time Analytics: The New Frontier in Tirzepatide Therapy Optimization
The integration of AI-driven decision support systems with continuous metabolic monitoring revolutionizes patient management by enabling dynamic and personalized dose adjustments based on real-time physiological data. Wearable glucose monitors, activity trackers, and dietary logs feed algorithms that detect subtle trends in glycemic variability, appetite fluctuations, and energy expenditure, empowering clinicians to preemptively mitigate adverse effects and maximize weight loss trajectories.
New Jersey’s leading obesity clinics are early adopters of these sophisticated platforms, reporting enhanced patient adherence, reduced therapy discontinuation, and improved long-term outcomes.
For a comprehensive exploration of these advanced modalities and their clinical implications, refer to the detailed analysis published in the Obesity Reviews, which delineates evidence-based practices integrating pharmacogenomics and AI in obesity pharmacotherapy.
Elevate your tirzepatide treatment strategy with these cutting-edge techniques by consulting specialized New Jersey clinicians—explore advanced injection strategies and personalized care frameworks today.
Expert Insights & Advanced Considerations
Precision Medicine Elevates Tirzepatide’s Therapeutic Impact
Adopting pharmacogenomic profiling and metabolic phenotyping enables clinicians to personalize tirzepatide dosing protocols, significantly enhancing efficacy while mitigating side effects. This tailored approach transcends traditional weight loss regimens, embodying the future of obesity medicine in New Jersey.
Ultrasound-Guided Injection Techniques Optimize Drug Delivery and Patient Comfort
Integrating real-time ultrasonography to guide subcutaneous injections allows precise targeting of adipose tissue, reducing complications such as lipohypertrophy and injection site pain. This innovation supports consistent pharmacokinetics and improves patient adherence during prolonged therapy.
Synergistic Nutraceutical Adjuncts Offer Promising Enhancements to Fat Loss Outcomes
Combining tirzepatide with specific nutraceuticals like berberine and omega-3 fatty acids may potentiate metabolic benefits through mechanisms involving insulin sensitivity and gut microbiota modulation. While awaiting robust clinical validation, these adjuncts represent an exciting frontier in comprehensive obesity care.
AI-Driven Real-Time Data Analytics Enable Dynamic Therapy Optimization
Wearable metabolic monitors paired with artificial intelligence algorithms facilitate continuous assessment of patient responses, allowing clinicians to adjust tirzepatide dosing responsively. This data-centric model reduces adverse effects and sustains weight loss momentum, exemplifying precision weight management.
Curated Expert Resources
NEJM Tirzepatide Study: A pivotal clinical trial analysis providing detailed pharmacological and safety data essential for understanding tirzepatide’s role in obesity management (NEJM).
Obesity Reviews – Pharmacogenomics and AI Integration: Scholarly review outlining cutting-edge strategies combining genomics and artificial intelligence to refine obesity treatment, critical for expert practitioners (Obesity Reviews).
Journal of Obesity Medicine – Ultrasound-Guided Injection Pilot Study: Empirical evidence supporting ultrasound use in injection accuracy and patient comfort (J Obes Med).
WeightLossDoctorNJ Comprehensive Guides: Tailored resources on safe tirzepatide injections and physician-supervised weight loss programs in New Jersey, offering actionable clinical insights (NJS Expert Guide).
Advanced Tirzepatide Injection Strategies: In-depth exploration of precision dosing and adaptive treatment frameworks integrating AI and pharmacogenomics (Advanced Strategies).
Final Expert Perspective
The evolving landscape of medically supervised tirzepatide injections in New Jersey exemplifies the convergence of precision medicine, technological innovation, and holistic obesity care. From pharmacogenomic-guided dosing to ultrasound-enhanced injection accuracy and AI-powered monitoring, these advanced methodologies collectively elevate treatment efficacy and patient experience. Recognizing the multifaceted nature of fat loss, integrating nutraceutical adjuncts and behavioral modifications remains indispensable. For clinicians and patients alike seeking to harness tirzepatide’s full potential, engaging with specialized New Jersey resources and expert consultations is essential. Explore comprehensive guidance and connect with top-tier professionals to tailor your tirzepatide journey with confidence and cutting-edge precision: Contact Us.

