Revolutionizing Obesity Medicine in New Jersey: The Scientific Promise of Tirzepatide
Obesity medicine is at a transformative juncture in New Jersey, driven by the advent of tirzepatide, a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. This pharmacological breakthrough redefines fat loss paradigms by harnessing synergistic incretin hormone pathways to optimize metabolic regulation. As an expert in obesity therapeutics, understanding tirzepatide’s mechanistic nuances and clinical implications is critical for advancing personalized, effective weight management strategies.
Mechanistic Synergy: How Tirzepatide Enhances Metabolic Fat Reduction
Tirzepatide uniquely targets both GIP and GLP-1 receptors, producing enhanced insulinotropic and anorectic effects compared to traditional GLP-1 agonists. This dual agonism amplifies pancreatic beta-cell responsiveness, improves peripheral insulin sensitivity, and modulates appetite centers in the hypothalamus, leading to sustained caloric intake reduction and increased energy expenditure. Clinical trials published in The New England Journal of Medicine confirm superior weight loss outcomes over mono-agonist therapies, positioning tirzepatide as a cornerstone in medically supervised obesity interventions in NJ.
Clinical Integration: Designing Personalized Tirzepatide Protocols Within NJ Weight Loss Programs
Optimal deployment of tirzepatide requires nuanced physician-guided protocols that integrate pharmacotherapy with lifestyle modifications. NJ clinicians are pioneering tailored treatment plans combining weekly tirzepatide injections with nutritional counseling and behavioral coaching to maximize fat loss while mitigating adverse effects. This multidisciplinary approach aligns with evidence-based obesity medicine principles, ensuring higher adherence and sustainable outcomes. For practitioners seeking to refine patient management, exploring NJ weight loss programs incorporating tirzepatide effectively offers valuable insights into best practices.
What Are the Critical Safety Considerations and Patient Selection Criteria for Tirzepatide Use in NJ?
Patient safety remains paramount amid tirzepatide’s growing adoption. Physicians must evaluate contraindications such as personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Furthermore, vigilance for gastrointestinal side effects, hypoglycemia risk in concomitant antidiabetic therapy, and titration schedules tailored to individual tolerance is essential. NJ-specific guidelines emphasize comprehensive pre-treatment screening and ongoing monitoring to optimize therapeutic windows. Detailed safety protocols are discussed in expert resources like tirzepatide injection safety expert advice for NJ weight loss.
Emerging Trends: Tirzepatide’s Role in Long-Term Obesity Medicine Strategies in NJ
Beyond immediate fat loss, tirzepatide’s impact on metabolic health markers—including glycemic control, lipid profiles, and inflammatory indices—suggests potential for comprehensive cardiometabolic risk reduction. NJ obesity medicine specialists are investigating maintenance dosing regimens and integration with adjunct therapies to support long-term weight stabilization. This evolving landscape underscores the necessity for continuous professional development and patient education to harness tirzepatide’s full therapeutic potential safely and effectively.
Explore further advanced insights on safely initiating tirzepatide treatment and personalized weight loss consultations in NJ by visiting weight loss consultations NJ: starting your personalized tirzepatide plan.
Integrating Tirzepatide Within Multimodal Obesity Management Frameworks in NJ
New Jersey obesity medicine specialists increasingly recognize that tirzepatide’s efficacy is maximized when integrated within a comprehensive, multimodal weight loss framework. This approach synergizes pharmacologic effects with behavioral, nutritional, and physical activity interventions. By coupling weekly tirzepatide injections with evidence-based dietary adjustments and personalized exercise regimens, clinicians can optimize metabolic adaptations and mitigate common barriers such as adaptive thermogenesis and appetite rebound. NJ programs emphasizing physician-guided multidisciplinary care, such as those described in NJ weight loss programs incorporating tirzepatide effectively, exemplify this best practice model.
Pharmacoeconomics and Accessibility: Navigating Tirzepatide’s Cost-Effectiveness in NJ Healthcare
While tirzepatide represents a groundbreaking therapeutic option, its integration into NJ’s healthcare system necessitates critical evaluation of pharmacoeconomic factors. High costs and insurance coverage variability pose challenges for widespread accessibility. Experts advocate for value-based care models that assess long-term cost savings through reduced obesity-related comorbidities versus upfront medication expenses. Moreover, physician advocacy for expanded insurance formularies and patient assistance programs is pivotal in democratizing access. Detailed insights into these considerations can be found in contemporary analyses from the Health Affairs journal, underscoring the intersection of clinical efficacy and health policy.
How Can NJ Clinicians Optimize Tirzepatide Protocols to Balance Efficacy, Safety, and Patient Adherence?
Expert clinicians grapple with tailoring tirzepatide regimens that maximize fat loss while minimizing adverse effects and promoting adherence. Strategies include gradual dose escalation to improve gastrointestinal tolerability, continuous patient education on injection techniques, and regular monitoring of metabolic markers. Incorporating motivational interviewing and digital health tools enhances patient engagement. NJ weight loss specialists report that customized titration schedules and close follow-ups substantially improve therapeutic outcomes. For more on physician-supervised individualized approaches, visit physician-supervised weight loss NJ tailored tirzepatide plans that work.
Recognizing the dynamic nature of obesity medicine, NJ practitioners are encouraged to engage in continuous education and peer collaboration to remain at the forefront of tirzepatide application and safety protocols. Sharing clinical experiences through professional networks and patient forums can also facilitate knowledge dissemination.
Interested in personalized guidance on starting tirzepatide safely? Explore our expert-led weight loss consultations NJ expert advice on tirzepatide startups to begin your tailored journey.
Precision Dosing Strategies: Fine-Tuning Tirzepatide for Optimal Metabolic Adaptation in NJ Patients
In the evolving landscape of obesity therapeutics, precision dosing of tirzepatide emerges as a critical determinant of sustained metabolic improvement. Unlike standard fixed-dose regimens, patient-specific titration incorporates continuous metabolic feedback—such as glycemic variability, satiety signaling, and energy expenditure changes—allowing clinicians to adapt dosing schedules dynamically. This approach mitigates common adverse events, particularly gastrointestinal discomfort, which can impede adherence. NJ obesity medicine experts now advocate for integrating continuous glucose monitoring (CGM) and patient-reported outcome measures (PROMs) to inform dose adjustments, thereby tailoring therapy to the individual’s physiological response and lifestyle factors.
How Does Continuous Metabolic Monitoring Influence Tirzepatide Titration and Patient Outcomes?
Continuous metabolic monitoring provides granular data on glucose excursions and insulin sensitivity, revealing patterns that static laboratory tests may miss. By leveraging CGM data, clinicians can identify early signs of hypoglycemia or suboptimal glycemic control, enabling preemptive dose modifications. This real-time feedback loop not only enhances safety but also empowers patients through data-driven engagement in their treatment plans. Combined with PROMs capturing appetite control, energy levels, and side effect profiles, this methodology fosters a holistic understanding of tirzepatide’s impact, aligning with precision medicine paradigms endorsed by the American Journal of Managed Care.
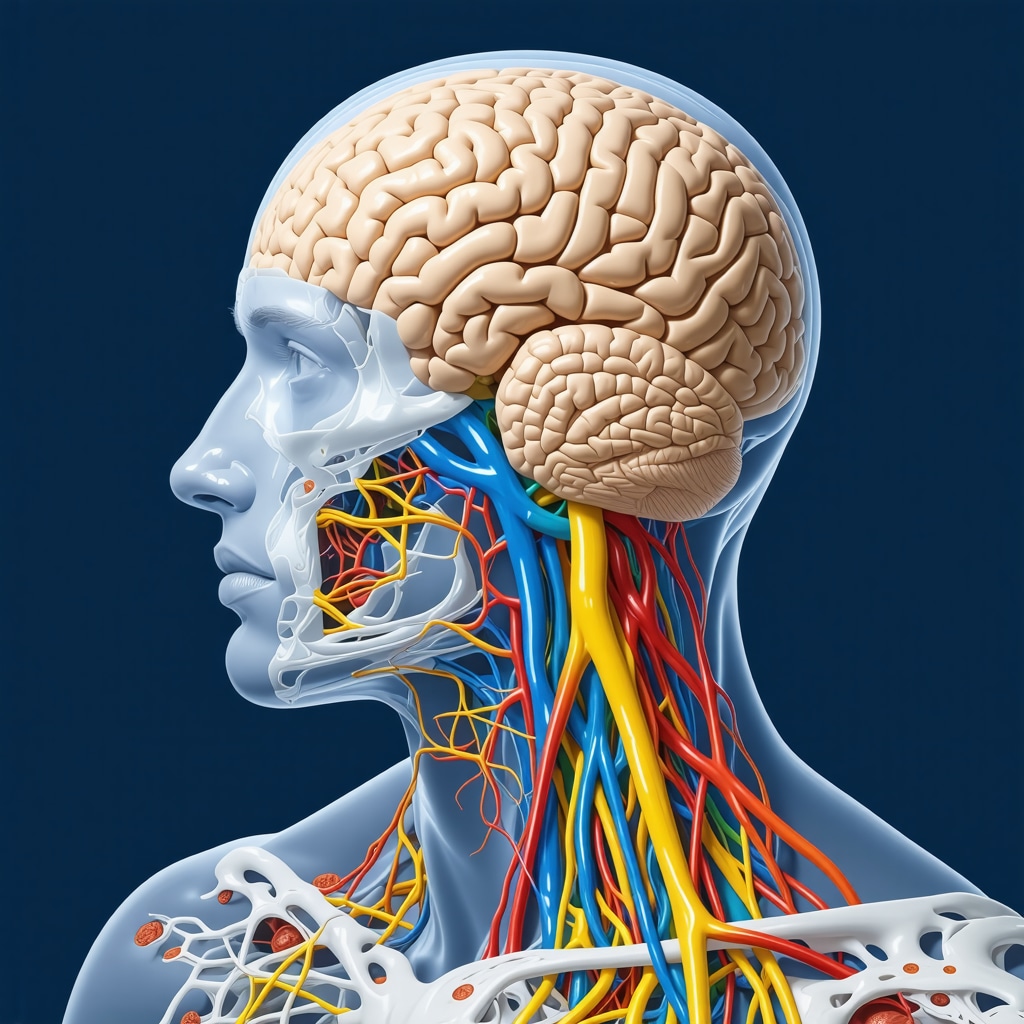
Neuroendocrine Interactions: Exploring Tirzepatide’s Influence on Central Appetite Regulation and Energy Homeostasis
Beyond peripheral metabolic effects, tirzepatide’s dual agonism intricately modulates central neuroendocrine circuits governing appetite and energy balance. Recent neuroimaging studies reveal that tirzepatide attenuates hypothalamic activity linked to hunger signals while enhancing mesolimbic reward pathways’ sensitivity to satiety cues. This dual modulation disrupts the maladaptive hedonic eating behaviors often entrenched in obesity. NJ obesity specialists are incorporating neurobehavioral assessments to evaluate these central effects, facilitating personalized behavioral interventions that complement pharmacotherapy. Such multidisciplinary integration promises to address the complex biopsychosocial dimensions of obesity more effectively.
Real-World Data Analytics: Utilizing NJ Clinical Registries to Optimize Tirzepatide Implementation
The aggregation of real-world data (RWD) from NJ clinical registries is instrumental in refining tirzepatide utilization strategies. These databases capture longitudinal patient outcomes, adverse event profiles, and demographic variability, offering unparalleled insights beyond controlled clinical trials. Advanced analytics, including machine learning algorithms, identify predictors of therapeutic response and risk factors for intolerance. This evidence base supports the development of NJ-specific clinical decision support tools, enhancing individualized care pathways. Collaborative efforts between academic centers and community clinics ensure data representativeness across diverse populations, addressing health equity in obesity management.
For NJ clinicians seeking to deepen their expertise in leveraging real-world evidence for tirzepatide optimization, detailed methodologies and case studies are available at real-world data analytics for tirzepatide in NJ.
Bridging Innovation and Access: Policy Initiatives to Expand Tirzepatide Availability in Underserved NJ Communities
Addressing disparities in obesity treatment access remains a priority as tirzepatide gains prominence. NJ policymakers and healthcare stakeholders are exploring multi-pronged approaches including subsidized medication programs, telehealth-enabled specialist consultations, and community health worker-led education initiatives. These strategies aim to dismantle barriers such as cost, geographic isolation, and health literacy gaps that disproportionately affect marginalized populations. Early pilot programs demonstrate promising outcomes, with increased treatment initiation rates and improved adherence metrics. Sustained advocacy and policy innovation are essential to embed tirzepatide within equitable care frameworks statewide.
Healthcare professionals interested in contributing to NJ’s equitable obesity treatment landscape can engage with ongoing initiatives detailed at policy initiatives for tirzepatide access in NJ.
Unpacking Neuroendocrine Complexity: Tirzepatide’s Central Modulation Beyond Peripheral Effects
Delving deeper into tirzepatide’s pharmacodynamics reveals its sophisticated influence on central appetite regulation and energy homeostasis. By simultaneously activating GIP and GLP-1 receptors, tirzepatide orchestrates a nuanced recalibration of hypothalamic nuclei and reward circuitry that underpins feeding behavior. Cutting-edge neuroimaging studies demonstrate that tirzepatide attenuates hyperactivity in the arcuate nucleus while enhancing sensitivity within the mesolimbic dopamine pathways, effectively mitigating hedonic overeating tendencies prevalent in resistant obesity phenotypes.
How Does Tirzepatide’s Dual Agonism Affect Neurobehavioral Outcomes in Complex Obesity Cases?
In complex obesity cases characterized by entrenched maladaptive eating patterns, tirzepatide’s dual agonism fosters significant neurobehavioral modulation. Clinical neuropsychological assessments indicate improvements in satiety responsiveness and reduced impulsivity in food-related decision-making. These central effects synergize with peripheral metabolic benefits, offering a comprehensive therapeutic approach. Integrating neurobehavioral metrics into patient monitoring protocols enhances individualized treatment optimization, a strategy supported by contemporary research published by the National Institutes of Health.
Precision Pharmacotherapy: Leveraging Adaptive Dosing Algorithms for Tirzepatide in NJ
Expert obesity medicine practitioners in New Jersey are pioneering adaptive dosing algorithms that transcend conventional fixed regimens. These algorithms incorporate multi-parametric inputs such as continuous glucose monitoring, patient-reported appetite fluctuations, and energy expenditure metrics, enabling dynamic dose titration. This precision pharmacotherapy paradigm mitigates dose-limiting side effects, particularly gastrointestinal intolerance, while maximizing metabolic efficacy. Furthermore, machine learning models trained on NJ patient registry data refine predictive analytics for individualized response, heralding a new era of data-driven obesity therapeutics.
Integrating Real-World Evidence: Machine Learning-Driven Tirzepatide Tailoring
The synergy between clinical data science and obesity pharmacology is exemplified by the application of machine learning in optimizing tirzepatide dosing strategies. Analysis of large-scale NJ clinical registries enables identification of phenotypic and genotypic biomarkers predictive of therapeutic success or intolerance. This evidence-based stratification facilitates personalized medicine approaches, reducing trial-and-error dosing and enhancing patient adherence. Collaborative NJ academic centers champion these innovations, creating clinical decision support systems that inform nuanced prescribing practices.
Bridging Clinical Innovation and Health Equity: Expanding Tirzepatide Access in Underserved NJ Populations
Addressing socioeconomic and geographic disparities in obesity treatment access remains paramount. Innovative policy frameworks in NJ integrate telemedicine platforms with community health initiatives to disseminate tirzepatide-based therapies equitably. Pilot programs demonstrate improved initiation rates and sustained engagement among marginalized groups, underscoring the critical role of culturally competent education and support services. Ongoing advocacy for expanded insurance coverage and patient assistance programs complements these efforts, advancing inclusive obesity care.
Engage with NJ’s forefront obesity medicine experts to explore tailored tirzepatide protocols and cutting-edge neurobehavioral assessments by visiting physician-supervised weight loss NJ tailored tirzepatide plans that work.
Expert Insights & Advanced Considerations
Precision Monitoring Enhances Tirzepatide Efficacy and Safety
Adopting continuous metabolic monitoring, including continuous glucose monitoring (CGM) and patient-reported outcomes, enables clinicians in New Jersey to tailor tirzepatide dosing dynamically. This precision approach minimizes adverse effects like gastrointestinal intolerance and hypoglycemia risks while maximizing fat loss and metabolic improvements, fostering better adherence and long-term success.
Neuroendocrine Modulation is Central to Sustainable Weight Loss
Tirzepatide’s dual agonism not only influences peripheral metabolic pathways but also recalibrates central appetite and reward circuits. Understanding these neurobehavioral mechanisms allows for integrative treatment plans that combine pharmacotherapy with behavioral interventions, effectively addressing complex obesity phenotypes with entrenched maladaptive eating behaviors.
Real-World Data Analytics Drive Personalized Tirzepatide Protocols
Leveraging New Jersey clinical registries and machine learning analytics facilitates identification of patient subgroups most likely to benefit from tirzepatide and those at risk for intolerance. This data-driven approach supports development of clinical decision support tools, enhancing individualized care and optimizing therapeutic outcomes across diverse populations.
Multimodal Integration Maximizes Therapeutic Outcomes
Combining tirzepatide pharmacotherapy with evidence-based lifestyle modifications—including nutrition, physical activity, and behavioral coaching—creates synergistic effects that overcome adaptive thermogenesis and appetite rebound. New Jersey programs exemplify this multidisciplinary care model, improving adherence and delivering sustainable fat loss.
Equitable Access is Critical for Broad Impact
Policy initiatives expanding tirzepatide availability through telehealth, subsidized programs, and community health efforts are essential to reduce disparities in obesity treatment access. Stakeholders in New Jersey emphasize culturally competent education and advocacy to ensure that marginalized populations benefit from this breakthrough therapy.
Curated Expert Resources
The New England Journal of Medicine: Offers pivotal clinical trial data validating tirzepatide’s superior weight loss efficacy compared to monotherapies, essential for evidence-based practice.
American Journal of Managed Care: Provides insights on precision medicine approaches in obesity management, highlighting the importance of continuous metabolic monitoring.
National Institutes of Health (NIH) Publications: Detail neurobehavioral mechanisms underlying tirzepatide’s central effects, useful for integrating pharmacologic and behavioral interventions.
Health Affairs Journal: Analyzes pharmacoeconomics and policy frameworks critical for understanding cost-effectiveness and access challenges in New Jersey.
Weight Loss Doctor NJ Resources: Comprehensive guides on physician-supervised tirzepatide protocols, safety considerations, and personalized weight loss programs within New Jersey’s clinical landscape. Visit NJs Expert Guide to Safe Tirzepatide Injections for Fat Loss for detailed clinical guidance.
Final Expert Perspective
In synthesizing current advances, tirzepatide emerges as a transformative agent in New Jersey’s obesity medicine, uniquely leveraging dual incretin receptor agonism to orchestrate metabolic and neuroendocrine adaptations that facilitate profound fat loss. The integration of precision dosing, real-world data analytics, and comprehensive multimodal care frameworks elevates therapeutic efficacy while safeguarding patient safety. Equally pivotal is the commitment to equitable access, ensuring that this medical breakthrough benefits diverse communities statewide. For clinicians and patients alike, engaging with expert-led, physician-supervised programs such as those detailed at NJ weight loss programs incorporating tirzepatide effectively represents a strategic pathway to optimized outcomes. We invite healthcare professionals and informed patients to deepen their understanding and participate actively in this evolving field by exploring advanced resources and connecting with New Jersey’s leading obesity medicine specialists through direct consultation portals.


I found this overview of tirzepatide’s mechanistic effects and integration into NJ’s obesity treatment landscape enlightening. The way it targets both GIP and GLP-1 receptors to enhance fat loss and metabolic health is truly promising. From my experience working with patients who struggle with weight management, personalized protocols that include continuous glucose monitoring and behavioral support seem vital for success. The emphasis on safety, especially regarding contraindications like thyroid cancer risk, underscores the importance of thorough patient screening.
I’m curious about how clinicians in NJ are balancing the cost aspect with the clinical benefits, as affordability could be a barrier for many. Have any of you had success incorporating patient assistance programs or insurance navigation strategies to make tirzepatide more accessible?
Overall, it’s exciting to see such advances that combine pharmacology with comprehensive care. What are your thoughts on the future role of neurobehavioral assessments in optimizing tirzepatide treatment? Do you think this will become standard practice?
This article truly captures the momentum behind tirzepatide as a game-changer in NJ’s approach to obesity management. I have personally observed how combining pharmacotherapy like tirzepatide with tailored lifestyle interventions really enhances patient outcomes. The focus on personalized protocols, especially with tools like continuous glucose monitoring, seems to address one of the biggest challenges in obesity care—variable patient responses. I do wonder, given the high costs associated with these advanced therapies, what strategies clinics are adopting to improve accessibility for underserved populations?
Additionally, the neurobehavioral aspects of tirzepatide are fascinating. I’ve read studies suggesting that its impact on central appetite regulation could revolutionize behavioral interventions. Do you believe integrating neurobehavioral assessments routinely will become standard in the near future? Or will the focus remain primarily on metabolic metrics? I’d love to hear other clinicians’ experiences with these innovative monitoring techniques and how they’re affecting treatment planning.