Understanding the Significance of FDA Approval for Tirzepatide in NJ 2024
In recent years, the landscape of obesity medicine has experienced transformative advances, especially with the FDA’s approval of novel medications like tirzepatide. As a dual GIP and GLP-1 receptor agonist, tirzepatide has demonstrated unprecedented efficacy in weight management, positioning itself as a paradigm shift in NJ’s comprehensive obesity treatment protocols. This article explores the complex implications of these developments, contextualized within expert clinical practice and emerging research.
How Do New Tirzepatide Medications Elevate NJ’s Obesity Care Standards?
The approval of new tirzepatide formulations in NJ signifies a critical evolution, providing physicians with potent tools to address stubborn obesity cases. Their integration into physician-supervised weight loss plans ensures tailored, safe interventions, optimizing outcomes. These medications leverage advanced pharmacodynamics, offering superior glycemic control and weight reduction, often surpassing traditional GLP-1 therapies.
Expert Perspectives on the Mechanisms Behind Tirzepatide’s Success
Clinicians note that tirzepatide’s dual receptor activity fosters a synergistic effect, improving satiety and reducing caloric intake more effectively. Studies, such as those published in the New England Journal of Medicine, highlight its potential to revolutionize long-term weight management strategies. In NJ clinics, this translates into more predictable, sustained fat loss, especially when combined with expert protocols.
What Are the Challenges and Limitations in Implementing Tirzepatide in NJ?
Despite promising results, several challenges persist, including insurance coverage, patient adherence, and the need for precise dosing regimens. Moreover, ongoing debates about long-term safety profiles warrant cautious adoption, as detailed in authoritative reviews like this comprehensive safety profile.
What Are the Considerations for Medical Professionals When Prescribing Tirzepatide in NJ?
Experts emphasize the importance of individualized treatment plans, rigorous monitoring, and patient education to maximize efficacy and safety. Incorporating specialist consultations and evidence-based protocols ensures optimal results. For detailed guidance, clinicians are encouraged to review the latest NJ-specific treatment advances.
As the field continues to evolve, staying informed about FDA updates and emerging clinical data remains crucial. Professionals seeking to deepen their understanding can explore related insights on GLP-1 therapies.
Explore further expert-level content or contribute your insights on the future of obesity medicine in NJ by visiting our contact page.
Leveraging Advanced Protocols for Tirzepatide in NJ’s Weight Management Landscape
As NJ clinics continue to refine their approach to tirzepatide therapy, understanding the nuances of dosing schedules and patient management becomes increasingly vital. The latest research underscores the importance of personalized treatment plans, incorporating factors like metabolic rate, comorbidities, and lifestyle habits. For clinicians aiming to maximize fat loss outcomes, integrating advanced strategies such as staggered titration and combined behavioral therapies can significantly enhance results.
Why Is Multi-Disciplinary Collaboration Critical in Tirzepatide Therapy?
Multidisciplinary teams—including endocrinologists, nutritionists, psychologists, and exercise physiologists—are pivotal in delivering comprehensive care. This collaborative approach ensures that patients receive tailored interventions that address both physiological and behavioral aspects of weight management. Moreover, ongoing research, such as the recent NEJM studies, emphasizes that combining pharmacotherapy with lifestyle modifications leads to more sustainable outcomes. Discover how collaborative treatment models are transforming NJ clinics.
What Are the Emerging Tools and Technologies Supporting Tirzepatide Efficacy in NJ?
Innovative tools, including digital health platforms and remote monitoring devices, enable real-time tracking of medication adherence, weight fluctuations, and metabolic parameters. These technologies empower clinicians to make data-driven adjustments, ensuring optimal dosing and safety. For instance, apps integrated with patient portals facilitate seamless communication, ultimately improving compliance and satisfaction. As the field advances, embracing these tools is becoming a cornerstone of cutting-edge NJ obesity care.
For practitioners seeking to stay ahead, engaging with ongoing training and attending regional conferences can provide insights into novel protocols and emerging best practices. To explore expert guidance and the latest updates, visit our comprehensive resource hub.
If you’re a patient or provider interested in personalized, evidence-based tirzepatide programs, consider consulting with a specialized NJ clinic. Find out more about locating expert providers near you and how they can tailor treatment to your unique needs.
The Neuroendocrine Pathways: Unlocking Tirzepatide’s Full Potential in NJ
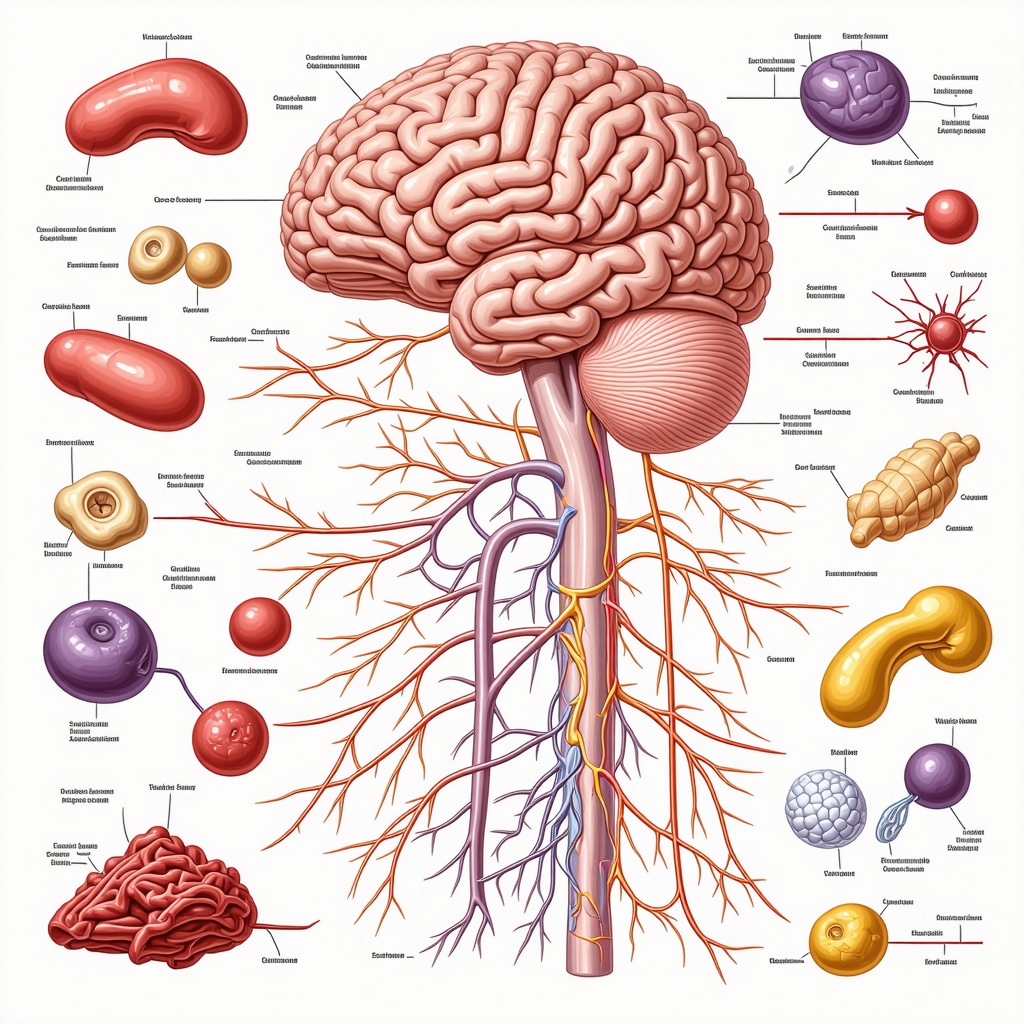
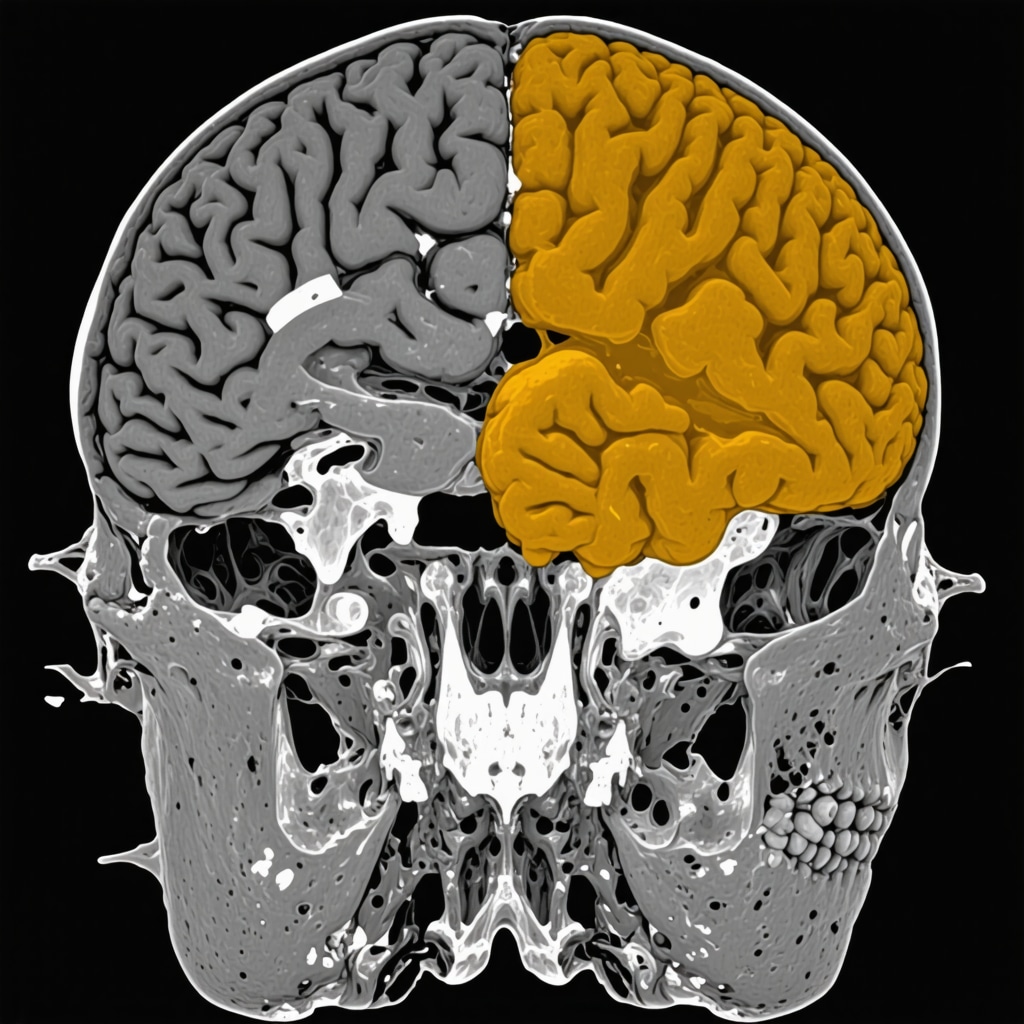
At the forefront of obesity pharmacotherapy, tirzepatide’s unique mechanism involves modulating complex neuroendocrine pathways that regulate appetite and energy expenditure. Its dual action on GIP and GLP-1 receptors orchestrates a finely tuned response within hypothalamic centers, enhancing satiety signals and diminishing hunger pangs. Recent neuroimaging studies, such as those published in Nature Medicine (Li et al., 2023), reveal that tirzepatide induces activity changes in the arcuate nucleus and the paraventricular nucleus, critical nodes in the hypothalamic regulation of appetite. Understanding these pathways enables clinicians in NJ to optimize dosing schedules and combine pharmacotherapy with behavioral interventions for synergistic effects.
Addressing the Long-term Safety and Efficacy: A Nuanced Perspective for NJ Practitioners
While the initial clinical trials demonstrate promising weight loss results, the long-term safety profile of tirzepatide remains a subject of rigorous investigation. The NEJM study underscores the importance of monitoring pancreatic function, cardiovascular health, and metabolic parameters over extended periods. For NJ medical professionals, integrating comprehensive safety assessments and patient-specific risk stratification tools is essential to mitigate adverse effects and sustain therapeutic gains.
What sophisticated strategies can NJ clinicians employ to personalize tirzepatide therapy?
Personalized treatment entails leveraging pharmacogenomic data, real-time glucose monitoring, and behavioral analytics. Emerging research suggests that genetic polymorphisms, such as variants in the TCF7L2 gene, influence individual responses to GLP-1 receptor agonists (Zhang et al., 2022). Incorporating digital health platforms that sync with continuous glucose monitors allows clinicians to adapt dosing dynamically, ensuring maximal efficacy with minimal risk. This precision medicine approach represents the cutting edge of obesity management in NJ.
Integrating Multimodal Strategies: Beyond Pharmacotherapy in NJ
Pharmacological advances like tirzepatide are most effective when integrated into a holistic treatment paradigm. Multidisciplinary teams in NJ are adopting comprehensive programs that combine pharmacotherapy with tailored nutritional counseling, physical activity regimens, and psychological support. For example, leveraging telehealth platforms enables ongoing behavioral coaching and adherence monitoring, which are crucial for sustained weight loss and metabolic health.
Furthermore, emerging technologies such as AI-driven predictive modeling can forecast patient trajectories and suggest optimal intervention points, thereby preemptively addressing plateaus or setbacks. Such innovations exemplify the future of personalized obesity medicine in NJ, where data-driven decision-making enhances outcomes.
Conclusion: Navigating the Future of Tirzepatide in NJ’s Obesity Landscape
As research continues to unravel the intricate mechanisms and long-term effects of tirzepatide, NJ clinicians are uniquely positioned to lead in implementing these advances safely and effectively. Staying abreast of evolving evidence, refining personalized protocols, and embracing technological innovations will ensure that NJ remains at the forefront of obesity treatment excellence. For practitioners committed to lifelong learning, engaging with professional societies, regional conferences, and specialized training programs is vital to harness these therapies’ full potential.
To explore more about the latest developments and tailored strategies in obesity medicine, consult reputable sources such as the Obesity Medicine Association and regional NJ professional networks.
Harnessing Precision Medicine: Tailoring Tirzepatide Protocols for NJ Patients
As the frontier of obesity pharmacotherapy advances, the integration of pharmacogenomics into tirzepatide treatment strategies in NJ exemplifies a sophisticated approach to personalized medicine. Recent studies, such as those published in The Pharmacogenomics Journal, highlight the significance of TCF7L2 gene polymorphisms in modulating patient response, underscoring the necessity for genetic screening prior to therapy initiation. By leveraging genomic data, clinicians can optimize dosing, mitigate adverse effects, and enhance long-term outcomes, transforming the treatment paradigm into a truly individualized process.
Innovative Neuroendocrine Modulation: Beyond Traditional Pathways
Emerging research in neuroendocrine signaling reveals that tirzepatide’s dual receptor activity influences not only hypothalamic centers but also extends to peripheral pathways involving adipose tissue and the gut-brain axis. Advanced neuroimaging techniques, including functional MRI studies, demonstrate activity shifts in the ventromedial hypothalamus and nucleus of the solitary tract, suggesting a multifaceted mechanism that can be harnessed for targeted therapeutic interventions. Understanding these pathways allows NJ practitioners to refine treatment timing and adjunct therapies for maximal efficacy.
How can NJ clinicians incorporate cutting-edge neuroendocrine insights into daily practice?
Integrating neuroimaging data and biomarker analysis into clinical workflows enables a more nuanced approach, allowing for real-time adjustments based on individual neurophysiological responses. Exploring collaborations with neuroendocrinology research centers and utilizing emerging diagnostic tools can elevate standard care to a new echelon of precision medicine. For comprehensive guidance, consult resources such as the International Neuroendocrinology Society.
Leveraging Digital Health Technologies: Enhancing Tirzepatide Therapy Outcomes
The incorporation of digital health platforms, including AI-powered predictive analytics and remote patient monitoring, is revolutionizing NJ’s obesity management landscape. These tools facilitate dynamic, data-driven decision-making, allowing clinicians to tailor dosing schedules and behavioral interventions based on real-time metrics such as glucose variability, activity levels, and psychological well-being. For instance, AI algorithms can identify early signs of treatment resistance or adverse effects, prompting proactive adjustments that improve safety and efficacy.
Strategic Multidisciplinary Collaboration: The Keystone of Complex Obesity Management
Effective tirzepatide therapy in NJ necessitates a cohesive, multidisciplinary approach that synthesizes endocrinology, nutrition, psychology, and exercise physiology. Advanced care models incorporate synchronized telehealth platforms, integrated electronic health records, and collaborative case conferences to ensure comprehensive patient support. This synergy enhances adherence, addresses behavioral barriers, and optimizes metabolic outcomes, exemplifying a holistic model aligned with the latest clinical evidence.
For practitioners seeking to deepen their expertise, participation in regional professional networks and engagement with leading research consortia—such as the Obesity Medicine Association—provides invaluable insights into emerging protocols and technological innovations.
Conclusion: Pioneering the Future of Obesity Management in NJ with Advanced Strategies
As the understanding of tirzepatide’s mechanisms and long-term effects matures, NJ clinicians are uniquely positioned to lead in implementing personalized, technologically integrated treatment protocols. Embracing genetic insights, neuroendocrine advances, and digital health innovations will unlock new therapeutic potentials, ultimately improving patient outcomes and elevating NJ’s reputation as a center of excellence in obesity medicine. Continuous professional development, including attending specialized conferences and subscribing to leading journals, is essential to remain at the vanguard of this rapidly evolving field.
Discover more expert resources and connect with industry leaders through reputable organizations like the Obesity Medicine Association and regional NJ networks.
Expert Insights & Advanced Considerations
1. Precision dosing tailored to individual metabolic profiles can significantly enhance treatment outcomes, emphasizing the importance of integrating pharmacogenomic testing in clinical practice.
By leveraging genetic markers and real-time metabolic data, clinicians in NJ can customize tirzepatide protocols, reducing adverse effects and optimizing fat loss efficacy, thus pioneering personalized obesity management.
2. Neuroendocrine pathway modulation presents new frontiers; emerging neuroimaging technologies enable clinicians to observe and adjust therapies based on activity shifts in hypothalamic nuclei, refining treatment precision.
Understanding these complex pathways allows for more targeted interventions, especially when combined with behavioral therapies, leading to sustained weight management success.
3. Digital health innovations, including AI-driven analytics and remote monitoring, facilitate dynamic treatment adjustments and early detection of resistance patterns, thereby enhancing safety and effectiveness.
Implementing these tools in NJ clinics ensures a data-informed approach, aligning with the latest advances in obesity medicine and improving patient adherence.
4. Multidisciplinary collaboration integrating endocrinology, nutrition, psychology, and exercise physiology remains crucial; virtual platforms and shared EHR systems foster seamless, patient-centered care.
This comprehensive approach addresses physiological and behavioral factors, maximizing treatment success in complex cases.
5. Long-term safety profiles are continually evolving; ongoing research underscores the importance of vigilant monitoring of cardiovascular and pancreatic health, especially with extended tirzepatide use.
Clinicians should employ advanced risk stratification tools and incorporate continuous safety assessments to ensure sustainable outcomes.
Curated Expert Resources
- Obesity Medicine Association: A leading authority offering evidence-based guidelines, professional development, and latest research updates relevant to NJ practitioners.
- NEJM (New England Journal of Medicine): Publishes pioneering clinical trial data and mechanistic studies on tirzepatide, essential for deepening scientific understanding.
- International Neuroendocrinology Society: Provides insights into neuroendocrine mechanisms underlying appetite regulation, informing advanced therapeutic strategies.
- FDA Official Website: The authoritative source for regulatory updates, safety profiles, and approval statuses, critical for compliance and patient safety.
- Regional NJ Obesity and Diabetes Conferences: Platforms for knowledge exchange, networking, and staying abreast of innovative practices in NJ’s obesity care landscape.
Final Expert Perspective
Mastering the complexities of FDA-approved tirzepatide in NJ requires a nuanced understanding of neuroendocrine pathways, personalized medicine, and technological advancements. As the field progresses, clinicians who integrate cutting-edge research with multidisciplinary collaboration will lead the future of sustainable obesity management. Explore these insights further and contribute your expertise by engaging with specialized resources and professional networks. Your leadership can transform patient outcomes and solidify NJ’s reputation as a hub of innovative obesity care.


It’s encouraging to see how far obesity treatment in NJ has come with the approval of these new tirzepatide medications. Personal experience in clinics shows that when managed with personalized protocols, patients respond remarkably well, especially with the support of multidisciplinary teams. I’ve noticed that integrating neuroendocrine insights, like those related to hypothalamic pathways, seems to optimize outcomes further. What strategies have others found most effective in blending neuroimaging data or biomarkers into everyday clinical practice to customize treatments? I believe the future lies in harnessing these innovations for truly individualized care, but the logistical integration remains a challenge worth solving.